Public health, policy, and pediatric optometry in modern practice (2000s–present)
By the time pediatric optometry entered the 21st century, it was already established as a specialty within the profession. What changed next was reach. Pediatric eye care moved beyond clinics and training programs and became part of larger public health conversations, insurance policy, and early-intervention efforts.
This is the point where pediatric optometry stops being something only professionals talk about and starts showing up in legislation, national programs, and everyday healthcare decisions.
Mandatory eye exams change access
One of the most influential developments came through state-level policy. In 2000, Kentucky became the first U.S. state to require a comprehensive eye examination for children entering school, rather than relying on basic vision screening alone (Zaba et al., 2003).
The results from early implementation were telling. A significant portion of children entering school were found to need glasses or follow-up care for conditions that had not previously been identified (Zaba et al., 2003). This reinforced what many optometrists already suspected: screenings alone were missing important issues.
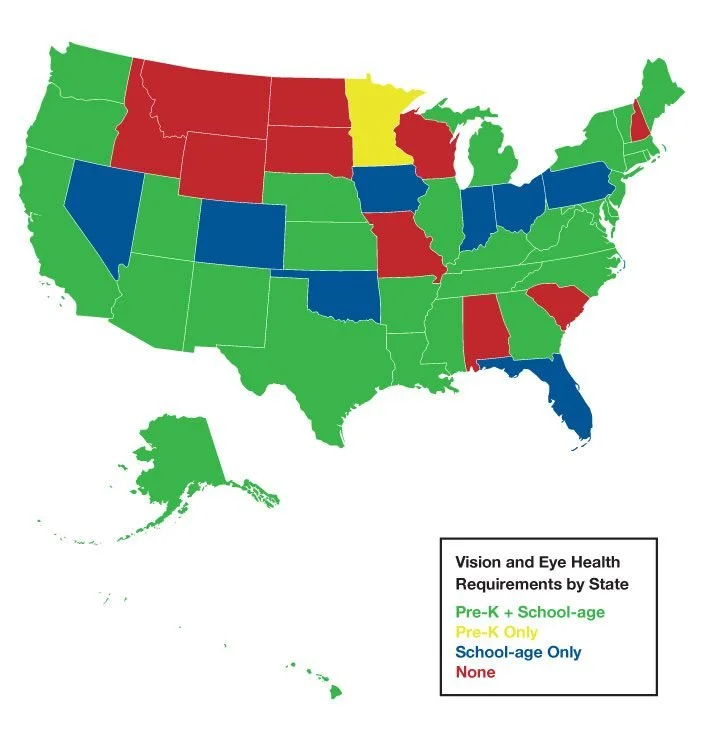
Following Kentucky’s example, other states introduced similar requirements or strengthened existing screening policies. While approaches still vary by state, these laws shifted how pediatric eye care was viewed. They were less optional and more expected.
Infant eye care enters the conversation
Another major change in the 2000s was the growing focus on infant vision. Historically, many parents (and providers) assumed eye exams weren’t necessary until children could read letters or entered school.
That assumption was challenged with the launch of InfantSEE® in 2005, a public health program developed by the American Optometric Association in partnership with Johnson & Johnson Vision and supported by former President Jimmy Carter (Palmer, 2023).
Through InfantSEE, optometrists volunteered to provide no-cost eye assessments for infants between 6 and 12 months of age. The response from the profession was huge – by the inaugural year, over 1,000 infants got free exams. Early program data showed that a meaningful percentage of infants examined had ocular or developmental findings requiring monitoring or referral (1 in 8) (Palmer, 2023). As of the latest figures, tens of thousands of infants have been seen through InfantSEE, and thousands of optometrists participate.
Insurance and federal policy matter
Policy changes at the federal level also reshaped pediatric optometry. With the passage of the Affordable Care Act (ACA), pediatric vision care was designated as one of the law’s Essential Health Benefits, requiring coverage for children’s eye exams and corrective lenses (Patient Protection and Affordable Care Act, 2010).
This shifted pediatric eye care from something families might delay or skip into something more routinely accessible. For optometrists, it meant pediatric patients were no longer a niche population but instead, they were a central part of primary eye care.
Myopia and modern pediatric challenges
In recent years, pediatric optometry has also had to respond to changing patterns in childhood vision. The rise in myopia (nearsightedness) worldwide has brought new urgency to pediatric care. Large epidemiological studies show increasing myopia prevalence among children and adolescents, particularly in urbanized environments (Holden et al., 2016).
As a result, pediatric optometry today often includes myopia management, increased attention to near work and outdoor time, and earlier monitoring of refractive development.
Additionally, I believe that children with special needs, such as autism or developmental delays, require specialized eye care. Today, optometrists are caring for children with increasingly diverse needs—including neurodevelopmental conditions, sensory processing differences, and complex medical histories—which requires flexibility in how eye exams are conducted and how care is delivered. This is a topic I am deeply passionate about, as I have also worked with these populations. I would love to explore this subject in more depth in a separate section (Under construction as I am still researching about it!).
Pediatric Optometry Community
There are now conferences and meetings specifically for pediatric and binocular vision specialists. The College of Optometrists in Vision Development (COVD) continues to advance knowledge in vision therapy and pediatrics. The American Optometric Association has a Sports and School Vision committee and other groups that focus on kids. And the American Academy of Optometry’s Pediatric/Binocular Vision Section regularly produces research (for example, large studies on amblyopia treatment that optometrists participate in alongside ophthalmologists) (Birch et al., 2021).
Conclusion
Looking back over the past century, pediatric optometry didn’t emerge all at once. It developed gradually in response to real needs, like schools noticing patterns, clinicians asking better questions, and families looking for answers when children struggled. What began with early screening programs and informal care eventually became a defined specialty built on training, research, and experience.
On a personal note, I’m excited about the future. Pediatric optometry will likely continue to expand with new research (perhaps genetics will play a role in predicting issues, or new therapies will emerge). There’s also a growing collaborative spirit – optometrists, ophthalmologists, pediatricians, educators, all working together on programs like InfantSEE or school eye health mandates!